Fighting Rising Healthcare Costs through Programming
Inflating healthcare costs have been a trending topic in medical, insurance, and employer conversations for many years. Despite high spending on healthcare in the United States, the life expectancy average is 78.8 years compared to a range of 80.7 to 83.9 in 10 other high-income, industrialized countries. Americans pay almost four times as much for pharmaceutical drugs as citizens of other developed countries, according to the Journal of the American Medical Association (JAMA). And, only 90% of the U.S. population has health insurance1.
Attributing to the increasing costs are a surprisingly small group of high cost claimants for most employer populations. A study by the Employee Benefit Research Institute (EBRI) found that generally, “20 percent of those insured by employer-based health benefits in the U.S. account for 80 percent of total spending on health care service” with a mere one percent accounting for 28 percent of total spending.
The study examined 5.8 million, employer-insured individuals that spent $38 billion on healthcare services in 2017 and found that the two percent of the population consistently spending the highest amount for healthcare services in 5 years accounted for 19 percent of total spending in 2017. The individuals had similar characteristics such as the presence of certain medical conditions like diabetes, hypertension, back problems/connective tissues problems, and respiratory diseases, and in most cases the claimants were the spouse of the insurance policy holder2.
Based on this data, it is not surprising to find the A&M System insured population of over 50,000 individuals mirrors these trends. Reports from Blue Cross and Blue Shield of Texas, the health insurance carrier for the A&M System, show that 5 percent of the current health plan population is diabetic (2,241 members), 15% of the current health plan population has hypertension (6,384 members), 20% of the current health plan population has both diabetes and hypertension (8,625 members), and 21% of the current health plan population has a musculoskeletal condition involving the back, knee, hip, neck or shoulder (12.932 members)3.
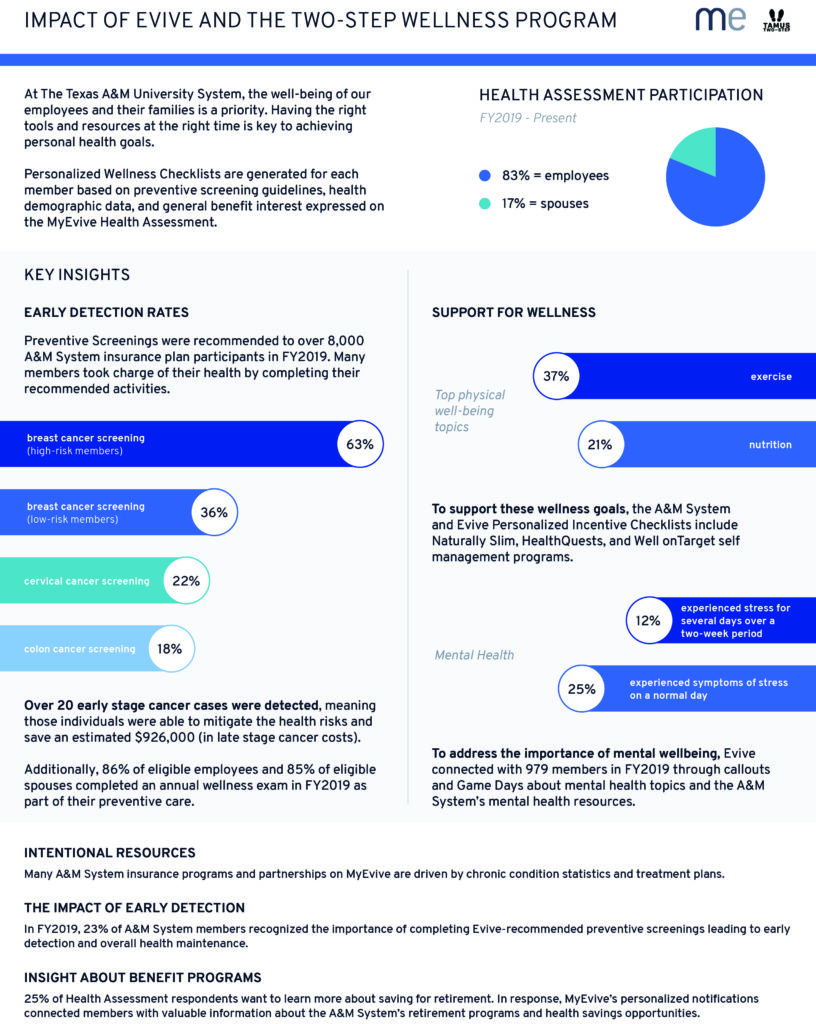
MyEvive also reported concerning health numbers on the MyEvive health survey that was applied as a wellness incentive credit activity in 2019. 58% of about 15,000 people completed the Heath Assessment and of those respondents, one-fifth self-diagnosed as having hypertension. 39% of respondents identified as having two or less of the indicators of metabolic syndrome, 4% said symptoms of a chronic condition held them back from doing day-to-day activities, and 24% would like to know more about nutrition.4 The infographic below provides more data about the A&M System population and its engagement with activities on the MyEvive checklists.
How A&M System Benefits Administration is responding
The EBRI confirms that cost-sharing is simply not enough to combat the rising costs of healthcare2. Industry experts encourage employers to help employees tackle conditions before they become high cost claimants through wellness programming. In 2018, the A&M System expanded its incentive-driven Wellness Program from employees completing a wellness exam for credit as had been the case for the last 4 years, to completing both the annual exam and the assessment survey. This encouraged employees to access MyEvive, which houses a plethora of benefit program resources, reminds employees about preventive screenings, chronic condition management, and other gaps in care. It also identified areas in the program which could be improved, such as an increase in access to nutritional resources and stress management.
In 2019, the program was again expanded to include more options and programs available to the A&M System-insured population, outside of preventive screenings. Employees were encouraged to take Well onTarget self-management courses, engage with Naturally Slim, or use a virtual service for behavioral health management.
Because the insurance plan has seen favorable results from these efforts and all-time high preventive screening adherence rates, premiums are remaining steady for full-time employees in FY2021, for the 5th year in a row. That is extremely uncommon in the medical insurance community today, with the exponential rising cost of healthcare. The wellness program is again expanding to include preventive skin care screening, nutritional counseling, and flu shots, combined with a new approach brought to us by some new vendor partners. The A&M System and Blue Cross and Blue Shield of Texas have partnered with Omada, Livongo, and Hinge Health to address chronic condition management for diabetes, hypertension, and musculoskeletal conditions in the A&M System insured population. These partners simplify treatment by using digital education and technology, making their programs easy-to-follow and more engaging for eligible individuals.
It is too early to tell if these continued efforts will drive costs down, but all signs point to “yes”. A&M System Benefits Administration continues to adjust wellness programming and insurance plan design to meet the needs of its insured population while maintaining a robust benefit package for everyone enrolled.
1- JAMA. “Health Care Spending in the United States and Other High-Income Countries.” https://jamanetwork.com/journals/jama/article-abstract/2674671
2-https://www.ebri.org/docs/default-source/ebri-press-release/pr-1254-highcostclaims-24oct19.pdf
3-This data is based on claims and provided to the A&M System Benefits Administration Office as aggregate, demographic data to protect the privacy of individuals according to HIPAA laws.
4-This data is based on aggregate data from an anonymous survey and individual details are not shared with A&M System Benefits Administration according to HIPAA laws. MyEvive Annual Report.
